Gardnerella Vaginalis: Signs, Symptoms & Treatment - HealthCentral.com
It's a tongue twister of a term, but an important one: Gardnerella vaginalis is the scientific name for a species of bacteria that lives inside your body, working alongside trillions of other microorganisms to keep your vaginal flora (that's code for the bacteria that typically live in and around your genitals) balanced and to ward off infection. But Gardnerella can sometimes go rogue and start multiplying too fast, contributing to a common reproductive health condition called bacterial vaginosis (BV).
Gardnerella Vaginalis
Frequently Asked Questions
How does a woman get gardnerella?
Gardnerella vaginalis is a type of bacteria that naturally exists in the vagina. When all systems are operating successfully, the bacteria play an important role in maintaining a healthy pH balance that protects the body from infections. But in some cases, Gardnerella vaginalis bacteria begin to multiply rapidly, leading to an imbalance of bacteria in the vagina, which in turn, causes bacterial vaginosis.
How long does it take for gardnerella to go away?
Gardnerella vaginalis is a type of naturally occurring bacteria in your body, so it won't ever "go away." It plays an important role in maintaining the pH balance in women's vaginas—in other words, it keeps people healthy. The infection that can be caused by too much GV is called bacterial vaginosis.
Is gardnerella an STD?
Gardnerella vaginalis is a type of bacteria. The infection it causes, bacterial vaginosis, is not considered a sexually transmitted disease, but many of its symptoms are similar to one. Experts do believe that sexual activity increases a person's risk for BV, but the exact correlation is not yet understood.
How did I get bacterial vaginosis?
Bacterial vaginosis is caused by an imbalance in vaginal bacteria. One of the leading causes of BV is a bacteria known as Gardnerella vaginalis. Bacterial vaginosis is not considered a sexually transmitted infection, but experts do believe that sexual activity raises the risk factor for developing it.
Around 30% of women will develop BV at some point during their pre-menopausal years, and some people are unlucky enough to get it on a recurring basis. BV is not technically considered a sexually transmitted infection, but it does share some of the same symptoms and risk factors as STIs (more on that later). Thankfully, because of its prevalence, BV is relatively easy to diagnose and treat.
What Is Gardnerella Vaginalis?
Wait, so is Gardnerella vaginalis bad for you? Not exactly. "Gardnerella vaginalis is a type of bacteria that can be found in the normal vaginal makeup," says Margaret Sullivan, M.D., OB/GYN at Tufts Medical Center in Boston. In limited quantities, Gardnerella is a good thing: It helps contribute to a balanced pH state—that's the measure of acidic versus alkaline that wards off bad bacteria from entering your vaginal tract.
But when Gardnerella vaginalis grows abnormally, it can disrupt your vaginal pH level and contribute to the vaginal infection known as bacterial vaginosis rather than protecting against it. The Gardnerella species was originally linked to BV back in the mid-1950s, and for many years, researchers believed it was the sole cause of this infection. "In the past, Gardnerella was believed to be the primary agent of bacterial vaginosis," Dr. Sullivan confirms. Doctors used tools like gardnerella DNA probes and vaginal pathogen tests (vag path for gardnerella) to measure the prevalence of Gardnerella and diagnose bacterial vaginosis. In the 70 years since that initial discovery, the scientific thinking has shifted. "The more recent thinking is that bacterial vaginosis is caused by a multitude of different bacteria, not just one," Dr. Sullivan says. Research shows that bacteria like Atopobium, Mobiluncus, and Prevotella (among others) also contribute to the development of BV.
While it used to be common practice to refer to BV as a Gardnerella vaginalis infection, you won't hear those terms used interchangeably nowadays. Instead, think of Gardnerella vaginalis as one of many bacteria that can lead to this common vaginal infection.

Gardnerella Vaginalis vs. Bacterial Vaginosis
Bacterial vaginosis is a treatable condition caused by an overgrowth of bad bacteria in your vagina. Gardnerella vaginalis isn't a condition in itself, but rather a species of bacteria that can contribute to the development of BV. Gardnerella is already present in your body in small amounts, but when it starts to multiply, it messes with your vaginal microbiome. This can lead to BV symptoms like pain, itching, and abnormal discharge.
To put it more simply: GV is a bacteria, and BV is a condition that can be caused by this bacteria.
Bacterial Vaginosis Symptoms
You won't always know if you have BV—in fact, as many as 84% of women have a totally asymptomatic case of this infection. But if you do have symptoms, here is what to look for: The most characteristic sign of bacterial vaginosis is a thin, grayish vaginal discharge with a strong "fishy" odor. The smell is often stronger after sexual activity and menses or anything that can increase the vaginal pH. BV can also cause itching and discomfort around your vulva and vaginal opening.
The odor is really what distinguishes BV from other types of vaginal conditions like yeast infections or STIs. "I tell patients that if they are having vaginal discharge that has an odor, itches, or is bloody, those would all be indications to get it looked at," Dr. Sullivan advises. "All things that itch are not yeast."
Still, for the average person, BV and yeast infections can be hard to tell apart. Here's a quick guide:
Bacterial vaginosis discharge: Thin, gray or green, strong fishy odor
Yeast infection discharge: Thick, odorless, "cottage cheese"-like look and texture
Of course, if you're uncertain, it's always worth seeing a doctor to get their opinion.
Bacterial Vaginosis Causes and Risk Factors
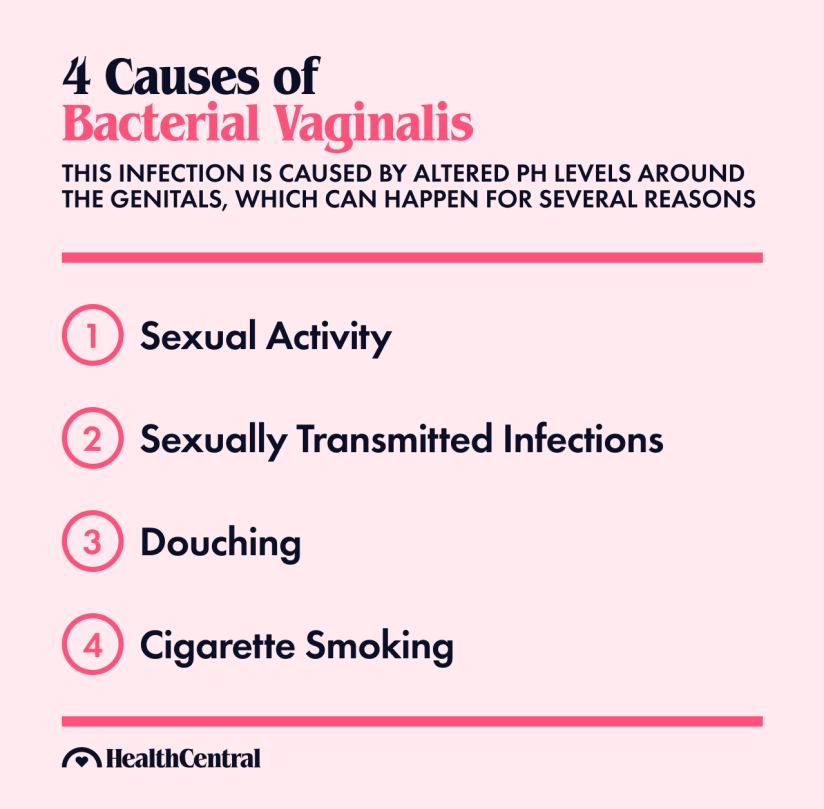
"Risk factors for BV include but are not limited to sexual activity, sexually transmitted infections, douching, and cigarette smoking," says Katrina Lee, M.D., an OB/GYN and assistant professor at University of Chicago. Really, anything that alters the pH levels in your vagina can act as a trigger for BV.
As for GV, there really are no "Gardnerella vaginalis causes," so to speak. This bacteria is naturally present in your vaginal flora and is healthy in limited quantities. When your vaginal pH levels are disrupted by sexual activity, douching, STIs, or incorrect vaginal hygiene, GV can grow abnormally and contribute to infection.
Is Bacterial Vaginosis an STI?
Bacterial vaginosis is not officially considered a sexually transmitted infection, but sexual activity does contribute to your risk—especially sex with a new partner or multiple partners. (Confusing, we know.) Part of why women get BV after intercourse is that semen is alkaline and thus makes the pH of the vagina increase, which then increases the susceptibility to BV. The part experts don't fully understand is why certain women get BV and others don't with the same circumstances.
And another thing: Women who have sex with women are at increased risk of developing BV and can sometimes (but not always) pass the infection to their partners. Men do not ever show symptoms of BV and don't need treatment for it, but it's not entirely clear whether or not they can spread it to a female sex partner. Using condoms, especially with a new or non-monogamous partner, can help lower your likelihood of getting or spreading BV.
Another reason to pay close attention to BV risk factors and symptoms: Leaving this infection untreated, especially on a recurring basis, can increase your risk for other reproductive health conditions. "Bacterial vaginosis increases susceptibility to sexually transmitted infections and preterm birth," Dr. Lee explains—including genital herpes, chlamydia, gonorrhea, and pelvic inflammatory disease. So, if you think you might have BV, it's worth getting it looked at ASAP. But if you're worried about asymptomatic infection, don't panic; most docs do not recommend treatment for asymptomatic BV.
Bacterial Vaginosis Diagnosis
You'll have to go to a doctor to get an official diagnosis for bacterial vaginosis. Traditionally, a medical provider will look at the vaginal discharge under a microscope and test the pH levels to determine the bacteria that might be present (including Gardnerella vaginalis and others). They may also outsource the swab testing to a lab, in which case you will get results back within a matter of hours or days.
Bacterial Vaginosis Treatment
BV treatment (or what was formerly and inaccurately known as Gardnerella vaginalis treatment) consists of a five- to seven-day regimen of antibiotics, prescribed either vaginally or orally. Metronidazole (Flagyl) and clindamycin (Cleocin) are two common options, prescribed as 150mg, 300mg, or 500mg tablets. Tinidazole may be prescribed as an alternative to Flagyl or Cleocin. Also, boric acid is sometimes used for recurrent infections.
Dr. Sullivan tends to prescribe vaginal application—a cream or gel that you put in and around your vagina—as it has fewer side effects than the oral version. With oral antibiotics, "there more systemic side effects," she explains, including an "upset stomach, diarrhea, and a metallic taste in your mouth." These medications aren't recommended for pregnant women, so let your doctor know if you are pregnant or trying to conceive. Other contraindications include certain blood dyscrasias and central nervous system diseases. An important side effect is intolerance to alcohol. Douching removes malodorous secretions temporarily but does not cure the infection (in fact, it may make you more susceptible to recurrence).
If someone has had at least three documented episodes of BV, Dr. Sullivan begins talking to them about a longer and more aggressive treatment plan called suppressive therapy. "We'll treat them a little longer than the usual five days—probably seven to ten days of the treatment dose, and then one to two nights a week for four to six months," she explains. "That resets everything in terms of the vaginal flora so the normal bacteria can take over from the abnormal bacteria." This reduces your chance of getting BV again in the future.

How to Prevent Bacterial Vaginosis
There is no foolproof way to prevent bacterial vaginosis, especially if you are sexually active. But here are a few tips to minimize your risk of getting it:
Limit your number of sexual partners, or if you do choose to have multiple partners, always use condoms. (This does double-duty of protecting against STIs, as well.)
Use gentle, pH balanced products around your vaginal area in the shower and avoid things like scented tampons and vaginal deodorants.
Don't douche. The vagina has the remarkable ability to clean and regulate itself, so you do not need to "clean" it with any additional fluids; this will only contribute to the imbalance of your microbiome.
Wear breathable underwear (cotton is a great choice) and change it daily.
If you'd like, you can try taking probiotics to support the health of your vaginal flora. Dr. Sullivan notes that while there isn't much scientific evidence to support this practice, many of her patients still say it works for them: "I do have patients who say they take probiotics and feel better," she says. "They feel like everything is more in sync when they take them."
If you do all these things and still end up with a BV infection, it's not the end of the world. Remember that this type of infection is super common. It happens, and it doesn't necessarily mean you're doing anything wrong or acting in an unhygienic way. Just make sure to see a healthcare provider for treatment as soon as you can.

Comments
Post a Comment