Sudden acquired retinal degeneration syndrome in a labradoodle
What Are Cataracts?
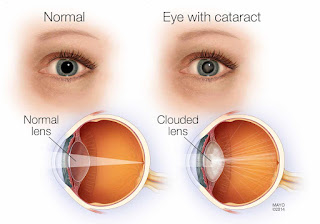
Cataracts are opaque or cloudy regions of the (normally clear) lens of the eye. Overall, about 24.4 million people in the United States are affected by cataracts, making this the most common cause of visual problems.
Older age raises your chances of developing this condition; more than half of people with cataracts are between 65 and 74 years of age. In addition, certain risk factors increase your risk of developing cataracts, including being assigned female at birth, having a family history of the condition, as well as certain health conditions, including diabetes, high blood pressure, obesity, and others.
Cataract symptoms can vary based on the type you have. It usually affects both eyes, causing clouded or blurry vision, loss of brightness in colors, and difficulty seeing at night, among other visual disturbances. Treatment options for cataracts range from making adjustments to your home environment to changing glasses or contact prescriptions to surgery. Fortunately, cataracts are highly treatable, with most people seeing improvements in their vision.
The lens of your eye, which sits behind the colored portion, or iris, is composed of multiple layers. Cataracts are categorized based on the layer of the lens that's affected. There are three major types: nuclear, cortical, and posterior capsular.
Nuclear CataractThis type occurs when there's clouding or discoloration of the inner, central part, or nucleus, of your lens. Nuclear cataracts tend to get worse gradually, affecting your long-distance vision more than your ability to see things close by.
Cortical CataractThe cortex of your lens is a layer that surrounds the nucleus. Cataracts here, known as cortical cataracts, tend to have a spoke-like appearance or look like drops of oil. They tend to spread from the edges of the lens toward the center. Glare from bright objects is a prominent issue if you have this type.
Posterior Capsular CataractA posterior capsular cataract occurs when the back (posterior) of the outer layer, or capsule, of your lens is affected. Extensive vision loss can happen if blurriness and discoloration affect the central part of the capsule. Common signs include experiencing glare and poor vision during bright light.
Generally, cataracts are a progressive issue, meaning you may not notice symptoms at first, but they get worse over time. Depending on your case, this can be a rapid or slow process, and there may be differences based on the type of cataract you have. One or both eyes may be affected.
The typical signs of cataracts include:
The lens of your eye is made of certain proteins, called crystallins, which are finely arranged to focus light to a layer of vision nerves (the retina) in the back of the eye. A cataract arises as the structure of these crystallins starts to break down, and they start to group together. The visual effects of cataracts occur as light entering the eye is scattered or altered by these groupings, which form into opaque or discolored patches.
Primarily, cataracts are the natural result of aging. As you get older, your body starts to lose its ability to remove waste and toxins and repair cells. In the lens of the eye, this natural progress causes the structure of the crystallins to be affected, and cataracts form. Genetics and other health factors or diseases may induce this process.
Risk FactorsAlongside older age, certain diseases, health conditions, and other factors increase your chances of developing cataracts. These include:
The primary goals of diagnosis are two see how severe the cataracts are and to make sure any symptoms aren't being caused by anything else. Diagnosis involves assessing your medical history, any medications you're taking, and a complete ophthalmic (eye) exam. Further testing may help rule out other eye conditions like glaucoma, chronic conjunctivitis, and diabetic retinopathy, among others.
Your healthcare provider (usually an optometrist or ophthalmologist, two types of eye doctors) may perform the following diagnostic tests:
Treatments for cataracts focus on restoring vision and clearing up any vision problems. Depending on the case, your provider may try non-surgical approaches before opting for cataract surgery.
Cataract SurgeryIf the cataracts are causing significant vision issues and getting in the way of your ability to read, drive, or perform daily tasks, your eye doctor may call for surgery. The primary surgical approach is called phacoemulsification. This surgery uses a device to transmit ultrasound waves via a small incision in the eye. These waves weaken the lens so it can be removed and replaced with an artificial lens (known as an intraocular lens or IOL).
Another approach is extracapsular surgery, which relies on a larger incision to remove the entirety of the affected lens. An IOL is then implanted in your eye, or contact lenses or special glasses can be used to correct vision.
Non-Surgical ApproachesWhile some cases of cataracts can't be prevented, making certain lifestyle changes and other measures may help. Prevention strategies include:
Certain eye and systemic health conditions are more likely to arise if you have cataracts. Such related conditions include both eye issues and those affecting other parts of the body. Vision problems often seen alongside cataracts include:
In addition to eye problems, systemic diseases also frequently accompany cataracts, including:
Worldwide, cataracts are the number one cause of preventable blindness, an issue that is more common in low to middle-income countries. That said, treatments are highly effective, with surgery having excellent results (prognosis) 70 to 80% of the time. Even with surgery, you may still require glasses or contacts to help you see.
Timely care and regular check-ups are critical in the management of cataracts. If you suspect you have cataracts or are experiencing vision problems impacting your ability to function independently, be sure to get your eyes checked. The sooner you get help, the better off you'll be.
How Much Does Cataract Surgery Cost?
Medicaid users may qualify for cataract surgery coverage, but the amount will vary from state to state. That's because vision care is considered an optional benefit, so state's can determine how much, if any, coverage to provide.
The National Academies of Sciences, Engineering and Medicine lists the vision benefits offered by each state's Medicaid program.
Funds available in health savings accounts (HSAs) and flexible spending accounts (FSAs) can help cover any out-of-pocket expenses, including a more expensive lens, according to both Dr. Olsen and Dr. Shakir. Certain charitable organizations, such as Mission Cataract USA and Operation Sight, also help provide free or low-cost surgery to those who can't otherwise afford it.
Before settling on a surgeon or facility, however, research how other patients rate their experiences, and use word of mouth to find an excellent eye surgeon in your area, advises Dr. Olsen. What's more, be aware of any extra costs that could come with follow-up visits and who you'll see during those visits, he recommends. Some ophthalmologists comanage their surgery patients with an optometrist at a different location.
"All of the costs associated with surgery and the care afterward should be very transparent," says Dr. Shakir. "Make sure you know ahead of time anything you're expected to [pay] out of pocket."
Another consideration: "A more expensive lens or technology may cost more up front but allow you to save money by not having to purchase eyeglasses or contacts," says Dr. Shakir. Your doctor will talk through all available options with you and their pros and cons to help you make the best decision about which IOL option will provide you with the range of vision you desire.
Nourish Your Eyes From The Inside Out
Eyetamins Vision Support contains the exact key ingredients shown by clinical studies to reduce your risk of long-term vision loss. Support your visual health and nourish your eyes from within with Eyetamins.
Does Medicare Cover Cataract Surgery Costs In 2023?
Cataract surgery is covered by Medicare Part B, which covers outpatient services. Most Medicare Advantage plans also cover cataract surgery, though you need to select a provider and facility that are in network with your specific plan.
Original Medicare covers 80% of the cost of cataract surgery, and patients are responsible for paying the remaining 20% (either out-of-pocket or with supplemental insurance) after meeting their yearly Part B deductible.
Medicare Advantage plans, however, may require a copay. Regardless, be sure to get a full rundown on your policy before booking any appointments. You can also use Medicare's procedure price lookup tool to get an idea of potential costs.
What Is the Best Medicare Plan for Cataract Surgery?Several Medicare Advantage plans cover all costs for cataract surgery, though you need to find a physician, hospital or surgery center that's contracted with your specific MA plan. To keep costs down, you may also want to seek an MA plan with low copays that includes vision insurance.
Most physicians and hospitals are contracted with Original Medicare, though not all are contracted with Medicare Advantage. You also need to pay for 20% of your procedure's total cost with Original Medicare.
You might consider a Medicare Supplement (Medigap) plan to bolster your basic Part B coverage. Plan G, for example, covers all cataract surgery costs, save for your Part B deductible and Medigap premium payments.

Comments
Post a Comment