Robert Zakar gives back to community
What Are The Best Eye Drops For People With Itchy Eyes?
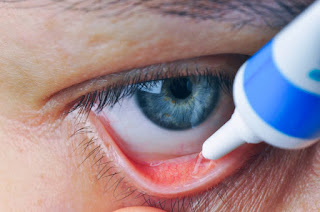
Eye drops may help to alleviate symptoms of itchy eyes. There are various over-the-counter and prescription eye drops. Examples include antihistamines, artificial tears, anti-inflammatory eye drops, antibacterial eye drops, and more.
An eye doctor called an ophthalmologist or optometrist can determine the cause and the best approach to treatment.
This article explores the causes of itchy eyes, the best treatments, including over-the-counter (OTC) and prescription eye drops, and when to consult a doctor.
A number of different eye conditions can cause itchiness, including:
Pink eyePink eye is also known as red eye or conjunctivitis. It refers to inflammation of the membrane covering the eye, and it can cause itchiness.
There are three kinds of conjunctivitis:
One type of allergic conjunctivitis is giant papillary conjunctivitis. This affects the inner eyelids and most often results from wearing contact lenses. Doctors recommend reducing the amount of time spent wearing contacts, and they may recommend a type of prescription or OTC medication called mast cell stabilizers.
Eye drops containing steroids may ease some severe cases of allergic conjunctivitis, but doctors generally only prescribe corticosteroids for short periods. An eye doctor will monitor the person for associated adverse effects, such as increased eye pressure.
Decongestant eye drops are available over the counter, but eye doctors do not recommend using them continuously, as doing so can cause "rebound" inflammation as soon as a person stops using them.
Topical antihistamines are safer to use for longer periods, as they can ease the body's response to allergens and reduce overall itchiness.
Dry eyeDry eye involves the body not making enough tears or tears to keep the eyes moist and comfortable. Common symptoms are stinging or burning sensations and frequent watering of the eyes. Treatments may include artificial tears that contain cyclosporine (Restasis) or lifitegrast (Xiidra).
Blepharitis is a condition that causes the eyelids to become irritated and swollen. A person may also notice crusty flakes on their eyelashes. The associated buildup of oil and flakes may lead to dryness and itchiness.
Treatment for blepharitis includes applying warm compresses and keeping the eyes clean and free of crust. A doctor may also prescribe an oral antibiotic, such as doxycycline.
Some other causes of dry eyes include:
Relieving the itchiness involves matching the medication to the underlying cause.
A person might choose one of the following prescription or OTC drop varieties:
Prescription
Over-the-counter
Eye drops that are free from preservatives, such as Freshkote, may be better for people who use eye drops frequently.
Eye allergies occur when the immune system reacts to an allergen in the environment. When an allergen comes into contact with antibodies in eye cells, the cells respond by releasing histamine. This reaction may cause tiny blood vessels to leak and the eyes to become itchy, red, swollen, and watery.
Millions of people in the United States alone have itchy eyes caused by allergies. Other symptoms may include an itchy and runny nose and a cough.
The following may trigger this type of allergic reaction:
If a mild reaction occurs only at specific times of the year, the issue is called seasonal allergic conjunctivitis. In North America, the symptoms may peak between April and May, when the pollen count in the air is higher.
Eye drops that contain antihistamines and decongestants can help manage the symptoms.
The following eye drops are available over the counter:
Others, available by prescription, include:
A doctor may recommend another approach, such as corticosteroids, immunotherapy, or treatment with medications called antileukotrienes. It is important to consult a healthcare professional before starting treatment with any new medication.
To prevent an eye allergy, doctors recommend people avoid the allergen as much as possible.
Factors to consider when choosing eye dropsTo determine the cause of the itchiness, a person's eye doctor might ask whether:
Having itchy eyes can be uncomfortable and may affect self-esteem or make a person reluctant to go outside, where there may be allergens. However, it should not affect vision.
If having itchy eyes is interfering with the quality of life, a person should contact a doctor.
Some causes, such as bacterial conjunctivitis, can sweep through environments such as schools. Anyone who has been exposed to the underlying pathogen needs treatment.
While some eye medications are available over the counter, it can be difficult to find the best option, and working with a doctor can help.
It is especially important to contact a doctor if there is a great deal of inflammation and redness in or around one or both eyes.
A range of eye conditions can cause itchiness. In some cases, allergens such as smoke, pollen, dust, dander, or fragrances are responsible.
Different medicated eye drops can treat different causes of itchy eyes, and a person may be able to access the right treatment over the counter. It is important to receive guidance from a healthcare professional before making a choice.
Can Covid-19 Actually Cause Pink Eye? Here's What An Ophthalmologist Says To Watch For
While life has slowly shifted away from peak pandemic times, Covid-19 continues to remind us in many ways that we still must be cautious. Most recently, a spate of pink eye cases has arisen in connection with a new subvariant of the virus. Currently, the new variant, XBB.1.16, a.K.A. "Arcturus", accounts for about 10 percent of Covid-19 cases in the U.S.
Pink eye is especially common in children, but can infection with SARS-CoV-2 really cause pink eye? Here's what you need to know.
What is pink eye?First, what actually is pink eye? Conjunctivitis, also known as pink eye, is an inflammation of the white areas of the eyes, known as the sclera, which can be caused by a variety of viruses and bacteria in our environments. In the case of viral pink eye, typically, both eyes will contract this condition, and it's contagious. Bacterial pink eye, which is also contagious, requires antibiotics for treatment.
Symptoms of viral pink eye are a burning sensation with watery discharge that may leave a crusty residue that could make eyelids stick shut. These symptoms usually accompany a runny nose, cough, or sore throat because the virus also affects the sinuses. This condition "can spread pretty easily," Ashley Brissette, an assistant ophthalmology professor at Weill Cornell Medicine and New York Presbyterian Hospital, tells Inverse.
In contrast, bacterial conjunctivitis can cause swelling and redness with a "milky" discharge, Brissette describes, though the eye might produce this icky stuff for only one night. While this type is also contagious, it typically stays limited to one eye.
Seasonal allergies can be another conjunctivitis culprit, making the eyes red, itchy, and watery.
Can Covid-19 cause pink eye?The SARS-CoV-2 virus that causes Covid-19 is a respiratory infection that affects the sinuses. The virus's proximity to the eyes can infect that part of the body too, Brissette says.
"We know that if the virus is in the sinuses, it's so close to the eye that you can get contamination, and then symptoms can start to present in the eyes," she says. Still, she notes that conjunctivitis is much more likely caused by adenovirus, which causes the common cold.
The connection between conjunctivitis and Covid-19 isn't new. Brissette harkens back to the old days of 2020 when we were all getting first acquainted with the novel disease. "There were eye manifestations even back in 2020 when Covid first presented," she says. About 1 to 3 percent of adults with Covid-19 presented pink eye as a symptom, according to the American Academy of Ophthalmology.
However, the pink eye doesn't automatically indicate that you have Covid-19. "If you have pink eye, it's probably more commonly related to adenovirus, which is a general kind of common cold virus that's in the environment," Brissette tells Inverse.
What if I think I have pink eye?There's no treatment for viral or allergy-induced pink eye, just as there's no treatment for the common cold. Brissette recommends frequent handwashing, using artificial tears to soothe red eyes (refrigerating the drops can make them feel more refreshing), and regularly changing face towels and pillowcases so viruses don't linger on surfaces that may touch others' eyes. Brissette tells her patients it can take two weeks for viral pink eye symptoms to quell.
Bacterial pink eye, on the other hand, does sometimes need to be treated. If severe enough, it can call for a round of antibiotic eye drops.
Brissette adds that if inflammation or blurry vision persists from either viral or bacterial infection, prescription eye drops can do the trick, though that rarely happens. "Oftentimes, the body just naturally heals it like it does for the common cold," she says.
The Covid-19 vaccine may also offer some extra protection, both against the virus and its comorbidities. "I think just having the vaccine will help to prevent your risk of development of Covid-19 and probably even decrease the severity of your symptoms," she says.
Above all, she says, "Good hygiene is essential."
more like this
Long Covid
These 12 Symptoms Can Probably Reveal If You Have Long Covid
Health
This Health Marker Will Reveal How Old Your Body Actually Is
Health
Researchers Found a Biomarker for Chronic Pain in the Brain
LEARN SOMETHING NEW EVERY DAYWhat To Know About The Recent Eye Drop Recalls
Two brands of eye drops were pulled from shelves in January and February after they were linked to a drug-resistant bacteria strain that has been found to have caused at least four deaths and serious health issues in several others. Weeks later, two other types of eye drops were recalled because they posed a different kind of contamination risk.
This flurry of recalls may have you second-guessing your trusted source of dry-eye relief, but there are significant differences among the recalls and plenty of steps you can take to stay safe.
"I would encourage all people out there who take eye drops to continue using them, of course making sure that they're not using any of these that are recalled," said Dr. Christopher Starr, a clinical spokesman for the American Academy of Ophthalmology.
Here's what to know about these recalls.
What eye drops have been recalled?In January, the Centers for Disease Control and Prevention and the Food and Drug Administration warned people to stop using EzriCare Artificial Tears and Delsam Pharma's Artificial Tears after the eye drops were linked to a drug-resistant strain of the bacteria Pseudomonas aeruginosa. Infections from this bacteria strain have caused at least four people's deaths, vision loss in 14 others and the surgical removal of four people's eyeballs.
Global Pharma, which makes EzriCare and Delsam Pharma's eye drops, recalled both products in February.
In March, a woman in Florida sued Global Pharma, claiming that an infection caused by the eye drops was so severe that doctors had to surgically remove one of her eyes.
The F.D.A. Has also warned people to stop using an eye ointment manufactured by Global Pharma because of possible contamination.
The manufacturer of EzriCare Artificial Tears said it was recalling the product out of "an abundance of caution."Credit...EzriCareThe two other eye drop recalls were not linked to the bacteria outbreak.
On March 1, Apotex recalled prescription eye drops used to reduce eye pressure in people with glaucoma or ocular hypertension. The company recalled six lots of Brimonidine Tartrate Ophthalmic Solution 0.15 percent because at least four bottle caps developed cracks, which could affect the product's sterility.
Apotex recalled six lots of Brimonidine Tartrate Ophthalmic Solution 0.15 percent prescription eye drops.Credit...Via F.D.A.On March 3, Pharmedica recalled two lots of Purely Soothing 15 percent MSM Drops because they were not sterile. These drops are used to treat eye irritation and swelling.
Pharmedica recalled two lots of Purely Soothing 15 percent MSM Drops because they were not sterile.Credit...Via F.D.A.Review the recall notices.The C.D.C. Said that, as of May 15, the drug-resistant bacteria strain linked to the recalled EzriCare and Delsam eye drops had been found in 81 people in 18 states.
The best way to find out if you have eye drops that were included in the recall is to review the recall notice provided by each company. Each notice has details on which batch of each product was affected.
The notice for the EzriCare and Delsam eye drops is here, and the notice for the Global Pharma eye ointment is here. The Apotex Brimonidine Tartrate notice is here and the Pharmedica Purely Soothing notice is here.
See a doctor if you have symptoms.People who have used these artificial tears and who have symptoms of an eye infection should see a doctor immediately, the C.D.C. Said. The symptoms can include yellow, green or clear discharge from the eye, redness of the eye or eyelid, increased sensitivity to light and eye pain or discomfort.
Apotex said that people who received its recalled eye drops, which were distributed between April 5, 2022, and Feb. 22, should contact their health care provider and pharmacy. The company also provided a phone number and website for people to request a "recall/return packet."
An Apotex vice president, Jordan Berman, said in an email that the company had seen only four bottles with cracked caps. He said that one of the bottles was from a customer or consumer complaint and the other three were found in retained samples — products that the F.D.A. Requires a company to keep back in case issues like these arise.
"There have been no drug safety reports related to negative health outcomes due to this product," Mr. Berman said.
Pharmedica said that, as of March 3, it had not received any reports of illness or other "adverse events" from the use of the eye drops. The company did not specify how many bottles were affected or how the bottles became not sterile.
Anyone who has issues with any of the recalled eye drops can file a report with the F.D.A. Online, by mail or by fax.
Eye drops are generally safe.Dr. Barbara Tylka, an optometrist at the Mayo Clinic in Rochester, Minn., said that, in general, eye drops are safe to use and that many people need them to treat conditions such as dryness or irritation. About 117 million Americans used eye drops and eyewash in 2020, according to Statista, a market research firm.
To use eye drops safely, Dr. Tylka said that people should use their own bottle and make sure it has not expired. People who have had eye drops prescribed to them for a procedure such as cataract surgery should stop using those products once the healing process is over, she said.
To safely apply eye drops, she said, people should use their nondominant hand to "gently tug on the lower eyelid, look up slightly," and then, with the dominant hand, put "that little drop in that lower cul-de-sac in the eyelid area."
Dr. Starr, an associate professor of ophthalmology at Weill Cornell Medicine, said that one thing some patients do wrong is press the bottle tip into the inner corner of the eye, which can contaminate the drops and scratch the surface of the eye. He said that when he accidentally hits his eyelid or eyelashes with the bottle tip, he considers the bottle contaminated and either resterilizes it or replaces it.
Dr. Starr and Dr. Tylka both emphasized that, while the recalls were worrying, eye drops are generally safe.
"I've continued to use eyedrops every day throughout this whole thing," Dr. Starr said.




Comments
Post a Comment