COVID-19 Can Cause Blepharitis in Your Eyelids
Cataracts And Diabetes: A Comprehensive Guide To Managing Eye Health In Diabetic Patients

Diabetes and cataracts are two common health issues that frequently coexist, providing special difficulties for those who have the disease. The eyes are one of the many organs that can be severely impacted by diabetes, a metabolic disease marked by elevated blood sugar levels. Cataract development is one of the most common eye complications among diabetic patients. In this article, Dr Brahmi Pandey, Cataract Specialist, Ophthalmologist and Medical Director, Balaji ENT and Eye Hospital shares the link between diabetes and cataracts.
"In diabetic patients, cataracts develop due to the accumulation of excess sugar in the eye's lens, causing protein denaturation and cloudiness," explains Dr Pandey.
Diabetic individuals are more prone to developing cataracts at an earlier age compared to non-diabetics. Studies indicate that the risk of cataracts is two to five times higher in individuals with diabetes.
There are different types of cataracts, including subcapsular, nuclear, and cortical cataracts. Diabetic patients may be at an increased risk of specific types, such as subcapsular cataracts.
Effects Of Diabetes On Eye HealthHigh blood sugar can affect your eyes in numerous ways. Here are some potential issues shared by Dr Pandey.
Diabetic Retinopathy
Apart from cataracts, diabetic retinopathy is another common diabetic eye complication. It involves damage to the blood vessels in the retina, leading to vision impairment or blindness if left untreated.
Also Read: Can Diabetic Retinopathy Be Reversed
Increased Risk of Glaucoma
Diabetic patients are also at an elevated risk of developing glaucoma, a condition characterised by increased pressure within the eye, potentially causing optic nerve damage.
Regular Eye Examinations
According to Dr Pandey, "Routine eye checkups is the first step for cataracts management. Diabetic individuals should undergo comprehensive eye exams at least once a year, including tests for intraocular pressure and a thorough examination of the retina."
Blood Sugar ControlMaintaining optimal blood sugar levels is paramount in preventing and managing cataracts in diabetic patients. Consistent blood sugar control can slow the progression of cataracts and reduce the risk of other diabetic eye complications.
Also Read: Do You Know Your Diabetes Type? Diabetologist Shares A Detailed Guide
Healthy Lifestyle Choices
Adopting a healthy lifestyle, including a balanced diet rich in antioxidants, regular exercise, and avoidance of smoking, can contribute to overall eye health. Foods high in vitamins C and E, zinc, and omega-3 fatty acids may be particularly beneficial.
Surgical Intervention
"In advanced cases of cataract, surgical removal might be the last option. Phacoemulsification, a modern cataract surgery technique, is often used, offering quicker recovery times and improved outcomes. Diabetic patients should discuss the potential risks and benefits with their healthcare team," shares Dr Pandey.
Collaborative Care
Effective management requires a collaborative approach involving endocrinologists, ophthalmologists, and other healthcare professionals. Integrated care can address both diabetes and its ocular complications comprehensively. Regular communication between healthcare providers ensures a holistic and tailored approach to each patient.
Also Read: 5 Essentials To Build Your Diabetes Management Toolkit
ConclusionIt is not merely about preserving vision; it's about safeguarding the essence of living—a life unhindered by the shadows of diabetic complications. There can be no conclusion to this but a beginning, where patients and healthcare providers should walk on a shared journey towards sustained well-being and clarity in sight, mind, and body.
People with diabetes can lessen their risk and experience cataracts by getting regular screenings, maintaining ideal blood sugar control, and making a commitment to a healthy lifestyle. Maintaining not only vision but overall well-being in diabetic patients requires a comprehensive approach that includes medical interventions, lifestyle modifications, and collaborative care. Finding your way in the complex terrain of cataracts and diabetes management requires regular communication and collaboration between patients and healthcare providers.
Eye Changes After Cataract Surgery Associated With Diabetic Retinopathy
Patients receiving uncomplicated phacoemulsification surgery for cataracts had greater increases in macular and choroidal thickness if they had early diabetic retinopathy without preoperative diabetic macular edema.
Greater increases in retinal superficial capillary plexus vascular density (SCP-VD), macular thickness (MT), and choroidal thickness (CT) occurred in patients with early diabetic retinopathy (DR) without preoperative diabetic macular edema (DME) compared with controls when they underwent uncomplicated phacoemulsification surgery for cataracts, according to a study published in Frontiers in Medicine.
Individuals with diabetes have been known to be 5 times more likely to develop cataracts,which can lead to blindness, compared with those without diabetes. Cataract surgery can be a risk factor for postoperative macular edema and secondary progression, however. This study aimed to assess the effect of cataract surgery on the macular microvasculature as well as MT and CT in patients with DR vs controls.
Female eye with long eyelashes close-upImage credit: Vladimir Voronin - stock.Adobe.Com
All patients included in this study had ophthalmologic examinations before participating in the study. This exam included best-corrected visual acuity (BCVA), intraocular pressure (IOP), and axial length (AL). For patients who had surgery in both eyes, the eye that was first operated on was used in the study. Patients were recruited from October 2020 to October 2022 from the Ophthalmology Department of Ruijin Hospital in Shanghai, China. Patients were included if they were 40 years or older, had a spherical diopter of less than –6 D, had an axial length of less than 26 mm, and had no history of intraocular surgery, DME and DR treatment, or glaucoma.
An optical coherence tomography (OCT) B-scan was done for all patients. Values for MT, CT, and SCP-VD were all provided automatically. All patients had phacoemulsification procedure with no complications.
There were 44 eyes from 44 participants who were included in the study, of which 22 were control eyes; the nonproliferative DR (NPDR) group had 13 men and 9 women, whereas the control group had 12 men and 10 women. Differences in age, sex, BCVA, IOP, and AL were not significant. In the NPDR group, 3 patients who had mild NPDR and 19 had moderate NPDR. All participants had an improvement in BCVA after surgery.
The DR group had no significant difference in foveal SCP-VD after operation but instead had an increase parafoveal SCP-VD at 1 and 3 months after the surgery compared with baseline, which was not found in the control group (mean [SD] fovea difference at 3 months, –0.17 [1.68%] vs 0.09 [2.3%]; mean [SD]parafovea difference at 3 months, 2.05 [1.35%] vs 0.77 [1.82%]). There was no significant difference in SCP-VD at any other time point.
The MT for patients in the DR group increased in all subfields at all 3 visits after surgery at 1 week, 1 month, and 3 months compared with the baseline. MT, measured in μm, had a significant change by the third month post operation compared with baseline in the fovea (34.86 [17.68] vs 17.23 [13.15]), the parafovea (22.55 [13.95] vs 11.69 [12.87]), and the perifovea (20.38 [16.81] vs 6.75 [6.21]).
CT increased at 1 week, 1 month, and 3 months after operation in the DR group for the fovea and 1 month and 3 months forthe parafovea. The changes in CT in μm were greater for the DR group at 3 months after surgery for the fovea (16.63 [13.38] vs 6.93 [15.29]) and the parafovea (15.34 [14.71] vs 6.51 [13.54]).
There were some limitations to this study. The sample size was small, although participants had varying degrees of retinopathy, ethnicity, and sex. The long-term effects on retina vessels could not be evaluated with the shorter follow-up period. The authors noted that a longer follow-up period would allow for assessment of the duration during which MT and CT would continue to increase as well as how that would affect the progression of DR.
The researchers concluded that uncomplicated phacoemulsification appeared to increase MT, SCP-VD, and CT for patients who had not had a prior surgery for DME and had mild or moderate NPDR compared with controls.
"However, the short-term postoperative visual prognosis of cataract patients with mild to moderate NPDR without preoperative DME is the same as that of healthy patients in this study," the authors wrote.
Reference
Yao H, Yang Z, Cheng Y, Shen X. Macular changes following cataract surgery in eyes with early diabetic retinopathy: an OCT and OCT angiography study. Front Med. Published online November 14, 2023. Doi:10.3389/fmed.2023.1290599
What Is A Nuclear Cataract?
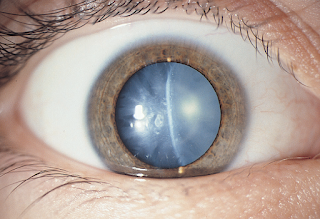
A nuclear cataract is a type of cataract that affects the center — nucleus — of the eye's lens. Typically, cataracts involve clouding or the opacification of the eye's natural lens, which can cause vision problems.
Cataracts are very common in older age. Over half of all Americans aged 80 or older have cataracts or have had surgery to treat them.
The eye's lens is responsible for focusing light onto the retina at the back of the eye and is located behind the colored part of the eye — the iris. When cataracts develop, the clear lens becomes cloudy, leading to various vision problems.
Doctors sometimes refer to nuclear sclerotic cataracts as nuclear cataracts. The term "sclerosis" refers to the hardening of body tissue. As these cataracts advance, the cloudiness may extend from the nucleus to other layers of the eye.
This article outlines the symptoms, causes, diagnosis, and treatment of nuclear cataracts.
A nuclear cataract specifically refers to a type of cataract that affects the nuclear region of the eye's lens, located in the center of the lens. The clouding or opacification of this central portion of the lens characterizes nuclear cataracts. These cataracts are associated with changes in the density and transparency of the lens nucleus.
Read about different types of cataracts.
Some of the symptoms associated with a nuclear cataract include:
Aging is the most significant and common factor contributing to the development of nuclear cataracts. The eye's lens contains water and proteins. The precise and orderly arrangement of these proteins maintains lens transparency.
As people age, these proteins in the lens undergo various structural and chemical alterations, becoming less stable. This instability can result in the aggregation and clumping of the lens's proteins within the central nucleus of the lens, leading to the lens's nucleus becoming cloudy and opaque.
Risk factors for nuclear cataracts include:
Diagnosing nuclear cataracts typically involves a comprehensive eye examination by an eye care specialist, such as an ophthalmologist or optometrist.
The eye doctor will use a slit-lamp biomicroscope, which provides a magnified view of the eye's structures, including the lens. This allows them to examine the clarity and condition of the lens, looking for signs of opacification or clouding associated with cataracts.
To get a better view of the lens and its internal structures, they may use dilating eye drops to enlarge the pupils temporarily. This allows for a more thorough examination of the cataract and its severity.
The treatment for nuclear cataracts typically involves surgical intervention. Cataract surgery is one of the most common and successful surgical procedures worldwide.
The treatment process typically follows these steps:
Genetics play a key role in people's likelihood of developing nuclear cataracts. However, several lifestyle and dietary practices may help reduce the risk of developing cataracts or slow their progression.
The outlook for people with nuclear cataracts is generally favorable if they have surgery. Cataract surgery improves visual acuity for around 95% of people.
Untreated cataracts can lead to gradual vision loss and even blindness, severely impacting a person's daily activities and quality of life. A 2023 systematic review and meta-analysis also found an association between visual impairment in older adults and an increased risk of dementia and cognitive impairment.
Here are the answers to some frequently asked questions about nuclear cataracts.
Is a nuclear cataract serious?Nuclear cataracts are a common age-related eye condition. While they can cause vision problems, doctors do not typically consider them a serious or life threatening condition. However, they can significantly impact a person's quality of life by affecting their vision.
Cataracts are highly treatable with surgery, which is an effective and safe procedure. Cataract surgery can restore clear vision and improve a person's quality of life.
What is the difference between a cataract and a nuclear cataract?A cataract is a general term that describes the clouding or opacification of the eye's natural lens, which can result in vision problems. There are different types of cataracts, and a nuclear cataract is one specific cataract subtype.
Nuclear cataracts are the most common type of cataract. They cause the center of the eye's lens to become cloudy, affecting a person's vision.
Several risk factors exist for nuclear cataracts, but older age is the most common.
Cataract surgery replaces a person's cloudy lens with a prosthetic intraocular lens and is safe and effective. Most people regain their vision after surgery. Without treatment, cataracts can cause vision loss.

Comments
Post a Comment