Swollen eyeball: Causes, symptoms, and treatments
Sinusitis Tied To Later Autoimmune Disease
A history of sinus congestion and drip may be a precursor to serious autoimmune disorders, a population-based study suggested.
Rates of rheumatologic conditions including antiphospholipid syndrome and Sjögren's disease were significantly higher in people with any experience with sinusitis, with odds up to seven times greater than in individuals with no such history, according to Vanessa Kronzer, MD, of the Mayo Clinic in Rochester, Minnesota, and colleagues.
For rheumatic diseases of any type, odds were increased 40% (OR 1.4, 95% CI 1.2-1.7) for those with a history of either acute or persistent sinusitis, the researchers reported in RMD Open.
Associations with specific rheumatic diseases were spotty, however. For ankylosing spondylitis, psoriatic arthritis, and most forms of vasculitis and rheumatoid arthritis (RA), only nonsignificant trends toward higher risk were found. And systemic lupus erythematosus trended in the opposite direction, with an odds ratio of 0.5 (95% CI 0.1-1.8).
As that broad confidence interval suggests, rates of many rheumatic disorders may have been too low to detect a real signal, despite more than 500,000 individuals being included in the study. Still, the authors felt the significant associations they did find are clinically relevant. "Overall, these findings point towards a role for sinus inflammation in the presentation, and possibly pathogenesis, of rheumatic disease," they concluded.
Why look for such an association? Kronzer and colleagues noted that previous studies had identified chronic exposure to "respiratory irritants," including tobacco smoke, airborne silica, and others as risk factors for various autoimmune diseases. Moreover, their own work had linked a suite of respiratory diseases (including sinusitis) with risk for RA. That led to the question of whether sinusitis by itself -- a relatively mild but very common condition -- might predispose toward rheumatic disease.
For the new study, the researchers drew on the long-running Rochester Epidemiology Project, with participation from most healthcare institutions in Olmsted County, Minnesota, the region surrounding the Mayo Clinic's headquarters. Detailed longitudinal data from more than half a million county residents were included.
Kronzer and colleagues focused on individuals with at least 7 years of medical history. They identified 1,729 people with incident rheumatic disease, with their "index date" counted as the first time their records indicated a rheumatic disease diagnosis. Each case was matched with three other people in the database for age at index date, sex, and approximate duration of medical records; 5,187 in total. Participants were counted as having a history of sinusitis if their records indicated such a diagnosis (with the relevant ICD-9 code) at least 1 year prior to their index date.
Only a few dozen people developed rheumatic disease in most categories. For example, there were just 22 cases of ankylosing spondylitis and 26 of antiphospholipid syndrome. The most common disease was RA, of which 688 cases were recorded.
A total of 48 potential associations were evaluated. For some diseases, certain subtypes were examined separately, such as seropositive versus seronegative RA; the researchers also looked for associations with acute versus chronic sinusitis.
Most of these 48 evaluations didn't reach statistical significance. The strongest link was for antiphospholipid syndrome, which, despite the small number of cases, produced an odds ratio of 7.0 (95% CI 1.8-27) for any type of previous sinusitis and 6.0 (95% CI 1.5-24) in relation to chronic sinusitis. Others included the following:
Also significant was the association for all cases of systemic disease in aggregate (including Sjögren's, antiphospholipid syndrome, lupus, and systemic sclerosis), with odds ratios of 2.2 for all sinusitis and 2.6 for chronic sinusitis. Acute sinusitis seemed very weak as a predictor of rheumatic diseases.
Of particular interest, the authors said, was that the associations were strongest when sinusitis occurred 5 to 10 years prior to first diagnosis of rheumatic disease.
Kronzer and colleagues speculated that these associations stem from infections, probably bacterial, that trigger both the sinusitis and the development of autoimmune reactions. They cited earlier studies indicating that "both Staphylococcus and more recently Corynebacterium were implicated in pathogenesis of ANCA-associated vasculitis, whereas Ruminococcus gnavus was associated with lupus nephritis, RA, and spondyloarthritis." The researchers also argued that this is consistent with the 5- to 10-year delay between sinusitis and rheumatic disease diagnosis, insofar as autoimmune pathology is usually detectable long before clinical symptoms become established.
"Therefore, future studies should replicate the observed association between sinusitis and rheumatic diseases, search for additional causative organisms, and determine whether preventing or treating sinusitis can prevent and/or treat rheumatic diseases," Kronzer and colleagues wrote.
Limitations to the study included the small number of incident rheumatic disease cases in the database, the reliance on administrative data, and the geographically and sociodemographically restricted sample. The researchers also acknowledged the potential for reverse causation, in which the presence of subclinical autoimmune disease might promote sinusitis. Unmeasured confounders could have been present as well.
John Gever was Managing Editor from 2014 to 2021; he is now a regular contributor.
Disclosures
The study was funded by grants from the Rheumatology Research Foundation and the NIH.
Kronzer declared that she had no relevant financial interests. Two co-authors reported relationships with pharmaceutical companies and other commercial entities.
Primary Source
RMD Open
Source Reference: Kronzer VL, et al "Association between sinusitis and incident rheumatic diseases: a population-based study" RMD Open 2024; DOI: 10.1136/rmdopen-2023-003622.
Please enable JavaScript to view the comments
Sinusitis Linked To 40% Heightened Risk Of Rheumatic Disease
The common inflammatory condition sinusitis is linked to a 40% heightened risk of a subsequent diagnosis of rheumatic disease, particularly in the 5 to 10 years preceding the start of symptoms, finds research published in the open access journal RMD Open.
The risks seem to be greatest for a blood clotting disorder (antiphospholipid syndrome) and a condition that affects the body's production of fluids, such as spit and tears, known as Sjögren's syndrome, the findings indicate.
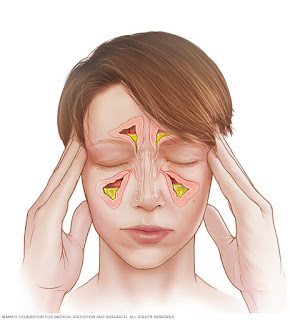
Sinusitis refers to inflammation of the lining of the sinuses, the small, air-filled cavities behind the cheekbones and forehead. And previously published research points to a link between various types of lung irritants, including air pollution and respiratory infections, and the development of rheumatoid arthritis, for example.
But it's not clear if sinusitis might also be a potential predisposing factor for other types of rheumatic disease. In a bid to plug this knowledge gap, the researchers carried out a case-control study.
They used data from the Rochester Epidemiology Project (REP), a medical records-linkage system of over 500,000 people resident in Olmsted County, Minnesota at some point between 1966 and 2014.
The study sample included 1729 adults, newly diagnosed with a systemic autoimmune rheumatic disease, such as rheumatoid arthritis, antiphospholipid syndrome, and Sjögren's syndrome; or vasculitis (blood vessel inflammation), such as giant cell arteritis (temporal artery inflammation) and polymyalgia rheumatica (muscle pain and stiffness).
Each of these patients (average age 63; two thirds women) was matched with 3 people (5187 in total) with no rheumatic disease, based on age at diagnosis and sex.
Cases of sinusitis before the diagnosis of rheumatic disease were divided into time segments of 1 to 5 years; 5 to 10 years; and 10 or more years.
Potentially influential factors were accounted for: age, weight (BMI), and smoking status at rheumatic disease diagnosis, sex, race and ethnicity.
The average time that elapsed between an episode of sinusitis and diagnosis of rheumatic disease was just over 7.5 years, with the most common diagnosis, rheumatoid arthritis (688) and polymyalgia rheumatica (610).
A history of sinusitis was associated with a 40% heightened risk of any new diagnosis of rheumatic disease, with the association strongest for systemic autoimmune rheumatic diseases, such as antiphospholipid syndrome–7-fold increased risk—and Sjögren's syndrome—more than double the risk.
Acute sinusitis was associated with an 18% heightened risk of seronegative rheumatoid arthritis (symptoms but no detectable antibodies).
The association between sinusitis and newly diagnosed rheumatic disease was strongest in the 5–10 years preceding symptom start, where the risk was 70% higher, overall, but 3-fold higher for Sjögren's syndrome and twice as high for polymyalgia rheumatica.
And the more frequent the episodes of sinusitis, the greater were the chances of a new rheumatic disease diagnosis. For example, those experiencing 7 or more were nearly 5 times as likely to be diagnosed with systemic autoimmune disease, nearly 9 times as likely to be diagnosed with Sjögren's syndrome, and twice as likely to be diagnosed with vasculitis.
Serial episodes of sinusitis without a previous history also showed a significant dose-response association with seronegative rheumatoid arthritis, rising to a quadrupling in risk for 5 or more episodes.
And overall, the association between sinusitis and rheumatic disease was strongest in people who had never smoked.
This is an observational study, and therefore no definitive conclusions can be drawn about causal factors. The researchers also acknowledge several limitations to their findings, including a predominantly White study population and few cases of certain types of rheumatic disease.
And reverse causation, whereby the rheumatic diseases themselves increase the risk of sinusitis, can't be ruled out, they add.
But bacterial pathogens, such as those involved in sinusitis, might have a role in rheumatic disease, added to which sinusitis is associated with speeding up artery hardening, lending extra weight to its potential inflammatory effects, explain the researchers.
And they conclude: "Overall, these findings point towards a role for sinus inflammation in the presentation, and possibly pathogenesis, of rheumatic disease."
Method of ResearchObservational study
Subject of ResearchPeople
Article TitleAssociation between sinusitis and incident rheumatic diseases: a population-based study
Article Publication Date27-Feb-2024
COI StatementJS has received research support from Bristol Myers Squibb and performed consultancy for AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, Pfizer and ReCor unrelated to this work. JMD has received research support from Pfizer, has licensed technology to Girihlet and Remission Medical and has provisional US patent application no. 63/243933 entitled, 'Methods and Materials for Assessing and Treating Arthritis'.
Disclaimer: AAAS and EurekAlert! Are not responsible for the accuracy of news releases posted to EurekAlert! By contributing institutions or for the use of any information through the EurekAlert system.
It Might Not Be Allergies: How To Tell If You've Got Chronic Sinusitis
People who've been suffering from allergies for a long time without relief might actually have chronic sinusitis, which requires a different treatment, a study has found. Hoping to help people get it addressed, the researchers have provided a list of signs and symptoms to watch out for.
Many, many people suffer from allergies, otherwise known as hay fever or allergic rhinitis (AR), experiencing symptoms that include sneezing, itchy nose, runny or blocked nose, itchy, red and watery eyes, and a cough. However, a new study by researchers at the University of Cincinnati (UC) has found that people who've thought they had allergies for years, in fact, had chronic sinusitis, a condition that, while similar to allergies in many respects, requires a different treatment.
"We've seen in our clinical practices many instances where patients have believed that they have allergies for many years and have sought treatment for allergies for years," said Ahmad Sedaghat, the study's corresponding author. "They have never found relief from their sinus/nasal symptoms because all along they've had [chronic rhinosinusitis or] CRS, an inflammatory condition of the sinuses."
The problem is that nasal allergies and sinusitis share overlapping symptoms, often presenting with a blocked nose or runny nose. And both can present with sinus pressure. But, despite their similarities, the two conditions have different treatments; treating sinusitis with allergy medication won't be effective.
Of the 219 participants who took part in the study, 91.3% were diagnosed with AR, but 45.2% were also diagnosed with chronic sinusitis. About half of the patients with sinusitis reported not being treated with intranasal steroid sprays, the first-line treatment for the condition.
Based on their findings, the researchers have determined that if someone has certain characteristics and symptoms, it should raise a suspicion that they may have chronic sinusitis instead of, or in combination with, nasal allergies. The following are strongly associated with chronic sinusitis and should prompt a visit to a medical professional:
Previous studies have shown that patients with poorly controlled chronic sinusitis have a significantly poorer quality of life, on par with conditions such as Parkinson's disease or coronary artery disease. They also have significantly greater antibiotic and steroid usage, and asthmatics also experience worsening lung health in association with poorly controlled chronic sinusitis. These studies highlight the importance of getting proper, and early, treatment for sinusitis.The researchers say that going forward, there should be an emphasis on education and raising awareness about chronic sinusitis.
"I hope that this study will give us the tools to raise awareness of CRS among the public, in particular the individuals at highest risk to suffer from CRS but not have it be recognized accurately," Sedaghat said. "I'm excited to be able to find a way to empower patients to think about the possibility of CRS, and I'm excited that we were able to do it in a way that will be very easy for patients. Overall, I believe our study will save and improve a lot of quality of life for patients."
The study was published in the journal Otolaryngology–Head and Neck Surgery.
Source: UC

Comments
Post a Comment