Goopy Eyes: Causes and Treatment
Ear Infection Treatment To Get Rid Of Symptoms

Ear infection treatments can vary based on which part of the ear is infected. This includes middle ear infections (otitis media), which cause inflammation in the air-filled space behind the eardrum, and outer ear infections (otitis externa), which cause inflammation in the external ear canal.
Although earache is the primary symptom of both middle and outer ear infections, the underlying cause can differ. The treatment will depend largely on whether the cause is viral, bacterial, or fungal and may involve pain medications, antibiotics, eardrops, or watchful waiting. Some cases can be treated with home remedies, while severe cases may require ear tubes to help drain fluids.
This article describes the various treatments for ear infections, including what to expect and what can be done if the treatments fail to clear the symptoms.
 © Provided by Verywell Health Illustration by Brianna Gilmartin, Verywell Can You Heal an Ear Infection Without Treatment?
© Provided by Verywell Health Illustration by Brianna Gilmartin, Verywell Can You Heal an Ear Infection Without Treatment? Middle ear infections often heal on their own without treatment. The same may be true for outer ear infections, but they generally take longer and are more likely to require treatment. The differences are due to how each type of infection develops.
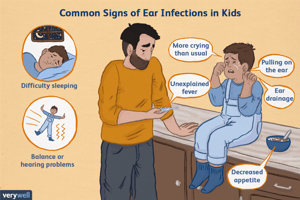
Middle Ear InfectionsOtitis media is more common in children than adults. Most cases are caused by an upper respiratory tract infection (URTI) like a cold or flu that causes the eustachian tube (the passageway connecting the middle ear to the back of the throat) to swell and fill with fluid.
Children are more often affected because their immune systems are less developed. Their eustachian tubes are also smaller and more horizontal, making it harder to drain fluid from the ear. Because of this, they can have recurrent infections, sometimes as many as four or five per year.
URTIs associated with middle ear infections are typically viral. These include rhinoviruses (the most common cause of colds), influenza virus (the flu), and respiratory syncytial virus (RSV). More often than not, the ear infection will clear once the viral URTI runs its course.
As a result, most middle ear infections don't need specific treatment and will usually clear within three to five days.
Related: What Causes Ear Infections?
Outer Ear InfectionsOtitis externa can affect both children and adults. It is popularly known as swimmer's ear because water remaining in the ear after swimming creates the ideal environment for bacteria or fungi to grow. The infection can also occur when a foreign object such as a cotton swab or ear plug introduces bacteria into the ear canal.
Because the moisture in the ear canal encourages bacterial and fungal growth, it often takes a while for the immune system to control the infection.
Without treatment, it can take several weeks rather than days for an outer ear infection to clear. The problem with this is that, when left untreated, the persistent inflammation can cause permanent narrowing of the ear canal and hearing loss.
Getting Over an Ear Infection With Treatment at HomeMany middle and outer ear infections can be treated quickly and effectively at home. This includes home remedies and over-the-counter (OTC) medications used to relieve inflammation, pain, and swelling.
Middle Ear InfectionsMany healthcare providers will take a watchful waiting, or watch-and-wait, approach with a middle ear infection, delaying antibiotics for two to three days to see if the infection clears on its own. Since kids often have recurrent infections, this helps lower the risk of antibiotic resistance (when pathogens like bacteria learn to defeat the drugs designed to kill them) caused by antibiotic overuse.
The at-home treatment of otitis media is mainly focused on pain relief. Given that most cases start as a URTI like a cold or flu, the treatment may include:
Aspirin Warning
Never give aspirin to children because it can cause a rare but potentially deadly reaction called Reye's syndrome. Cough and cold medicines are generally avoided in children under 4 years unless recommended by a healthcare provider.
In addition to OTC medications, rest and plenty of fluids can help resolve the underlying URTI.
Additional home remedies that can help include:
The treatment of swimmer's ear primarily involves ear drops. Several OTC options either acidify the ear canal (making it hostile to bacteria or fungi) or dry the ear canal (removing the moisture that promotes bacterial or fungal growth).
Options include:
Ear drops are usually applied three or four times daily for five to seven days. Instructions vary, so speak with your pharmacist or healthcare provider to ensure you are using them correctly.
Some people also swear by homeopathic ear drops containing belladonna (Atropa belladonna) or wolfsbane (Aconitum napellus), both of which are popularly used to treat earaches.
In addition to ear drops, OTC pain relievers like Tylenol, Advil, or Aleve can help ease ear pain.
Related: How to Use Ear Drops Correctly
Getting Over an Ear Infection With Antibiotic TreatmentOral antibiotics may be prescribed for middle ear infections that do not resolve on their own. Antibiotic or antifungal ear drops may be used to treat outer ear infections, while corticosteroid (steroid) ear drops can help ease inflammation and pain.
Middle Ear InfectionsAccording to guidelines from the American Academy of Pediatrics, a watchful-waiting approach is preferred in most children with acute otitis media. This is because four out of five children with otitis media will get better without antibiotics.
Antibiotics are typically reserved for:
In such cases, the recommended first-line treatment is high-dose Amoxil (amoxicillin) prescribed as follows:
Middle Ear Infections in Adults
Middle ear infections in adults are less common but often more serious due in part to underlying risk factors (like smoking or compromised immunity) that give rise to complications like mastoiditis (a type of skull bone infection) and permanent hearing loss.
Because of this, otitis media in adults is more often treated with antibiotics than not. The recommended treatment is Augmentin (amoxicillin and clavulanate) taken every 12 hours for 10 days.
Outer Ear InfectionsAlthough otitis externa can often be treated with OTC ear drops, prescription ear drops may be needed for the infection. These are often prescribed for people who have swelling and obstruction of the ear canal.
Antibiotic ear drops used for otitis externa are sometimes combined with a corticosteroid like hydrocortisone that helps ease inflammation. Options include:
If the infection is confirmed to be caused by a fungus, it can be treated with a 1% clotrimazole solution available over the counter. Prescription antifungal options include:
In most cases, you will need to use the ear drops for 10 to 14 days.
If there is ear swelling that blocks the ear canal, your healthcare provider may need to insert a tiny sponge into your ear canal called a wick. Applying the drops to the wick allows the medicine to be drawn into the ear canal beyond any areas of inflammation. Ear wicks can be left in place for two to three days and replaced with fresh ones if needed.
When Not to Use Ear Drops
You should avoid using ear drops—particularly over-the-counter ear drops—if you think you have a ruptured eardrum. Symptoms include sudden hearing loss, ear pain, ringing in the ears, ear drainage, and vertigo (spinning sensations).
There are ear drops like Floxin Otic that can be prescribed if your eardrum is punctured, but these should only be used under the direction of a healthcare provider. Other ear drops can be toxic to the middle ear, injuring the hearing bones (ossicles) as well as the eustachian tube.
Ear Infection Treatment Not WorkingIn an ideal situation, an ear infection will clear on its own or with a short course of medications. But this is not always the case, and some acute infections can resist treatment and become chronic.
An ear infection is considered acute if it lasts for up to six weeks and chronic if it recurs three times or more in a six-month period or four times a year.
Depending on the symptoms, there are several ways a healthcare provider can deal with a chronic ear infection.
Middle Ear InfectionsIf a middle ear infection does not respond to treatment, a tympanostomy tube (ear tube) may be needed to drain fluids and promote healing. These are typically used for people with recurrent middle ear infections or a long-lasting complication called serous otitis media in which fluid remains in the middle ear even after the infection has cleared.
Tympanostomy tubes improve hearing and also prevent recurrent infections and the overuse of antibiotics.
Tympanostomy tubes are placed under local anesthesia using a thin scope (called a transcanal endoscope) that directs the placement of the 2-millimeter tube in the eardrum. Once inserted, the tube is left in place until it falls out on its own, usually within four to 18 months. The hole will usually close on its own.
MastoiditisMastoiditis is a rare bone infection usually caused by severe untreated otitis media or otitis externa. It affects part of the skull called the mastoid bone located just behind the ear. Symptoms include ear pain, fluid discharge, hearing loss, and a visible swelling behind the ear.
Mastoiditis is a serious condition that often requires repeated or long-term treatment, This typically starts with intravenous (IV) antibiotics (delivered into a vein) followed by a course of oral antibiotics.
If the antibiotics do not work, a surgery called a mastoidectomy may be used to drain fluids by removing part of the mastoid bone. Ear tubes are also frequently part of the treatment plan.
Malignant Otitis ExternaRarely, an outer ear infection can spread into the floor of the ear canal and the bones of the base of the skull. This happens most often in people with a weakened immune system, including those with diabetes or who are undergoing chemotherapy.
Symptoms include ongoing drainage from the ear, ear pain, trouble swallowing, and weakness of the facial muscles. The infection can damage bones, tissues, and nerves and is life-threatening. It requires hospital admission and intravenous antibiotics, followed by long-term antibiotics and monitoring.
How to Prevent Ear Infections
Ways to reduce the risk of ear infections in you or your child include:
The treatment of an ear infection will vary by the location and underlying cause of the infection. Middle ear infections (otitis media), most common in children, often clear on their own. Infections that are severe or don't clear may require antibiotics. Children under 6 months are commonly treated whether symptoms are severe or not. While middle ear infections in adults are less common, they can be more severe and, more often than not, require antibiotic treatment.
Outer ear infections (otitis externa), common in adults and children, are mainly treated with ear drops. These include over-the-counter ear drops that are mildly acidic or reduce moisture in the ear canal. Outer ear infections may require prescription ear drops containing an antibiotic, antifungal, or corticosteroid drug.
10 Effective Earache Remedies
Not all ear infections are bacterial or need prescription medication. You may be able to relieve ear pain with home remedies or over-the-counter medications.
Earaches can be debilitating, but they don't always warrant antibiotics. Prescribing guidelines for ear infections have changed in the last five years. Your child might not even be prescribed antibiotics.
In fact, you could find all the relief you need in your home with treatments such as:
Here are 10 home remedies and over-the-counter treatments for earaches.
The following 10 remedies may help you relieve your pain. That said, treatment can depend on the cause, so you may want to see your doctor first.
1. Over-the-counter pain relieversYou can use over-the-counter (OTC) pain relievers like ibuprofen and acetaminophen to control pain associated with a painful type of ear infection called acute otitis media (AOM).
They're safe to use with or without antibiotics, but be sure to follow the dosing instructions on the label. These medications can also help lower a fever.
Talk with your doctor about the appropriate dose for children. Children and infant versions are available for many OTC pain relievers. It's unsafe for children under age 16 to take aspirin.
2. Cold or warm compressesPeople often use ice packs or warm compresses, like a heating pad or damp washcloth, to relieve pain. The same can be done for ear pain. This method is safe for both children and adults.
Place the ice pack or warm compress over the ear and alternate between warm and cold after 10 minutes. If you prefer either cold or warm, you can use just one compress.
3. Olive oilOlive oil has some antibacterial properties, though there's no solid scientific evidence to prove that drops of olive oil in your ear canal can soothe ear pain. That said, putting a few warmed drops of olive oil in the ear is safe and may be worth a try.
It's still a good idea to discuss this method with your doctor first, especially for children. Make sure the olive oil is no warmer than your body temperature by using a thermometer. This will help you avoid burning the eardrum.
4. Naturopathic dropsNaturopathic ear drops are made from herbal extracts. They can be found online and in some drug stores. An early study found that drops containing herbal extracts in a base of olive oil could be just as, or even more, effective as traditional OTC ear drops.
An old 2001 study found that using these drops may lead to improvement in ear pain levels. That said, a 2019 study suggests that they don't necessarily help when it comes to treating ear infections.
5. Chiropractic treatmentIf you go to the chiropractor for adjustments, you may find that your appointment can soothe your earache as much as your back pain.
There aren't many studies looking at the effectiveness of this. One older 2011 study suggests it may help, though how it works isn't understood. The effectiveness will also depend on the cause of your pain, so it's a good idea to see a doctor first for a diagnosis.
6. Sleep without putting pressure on the earSome sleep positions will aggravate pain from ear infections, while some can help relieve it. Sleep with the affected ear raised instead of having it faced down toward the pillow. This can help the ear drain better if necessary.
You can also sleep with your head elevated by using extra pillows. This can also help the ears drain faster.
7. GingerGinger has natural anti-inflammatory properties that can help soothe pain from earaches. Apply ginger juice or strained oil that was warmed with ginger in it around the outer ear canal. Do not put it directly into the ear.
8. GarlicGarlic has both antibiotic and pain-relieving properties. Soak crushed garlic for several minutes in warm olive or sesame oil. Strain the garlic out and apply the oil to the ear canal.
9. Hydrogen peroxideHydrogen peroxide can be used as a natural remedy for earaches, particularly if the cause is wax buildup. To use this method of treatment, place several drops of hydrogen peroxide into the affected ear. Let it sit for several minutes before letting it drain into a sink. Rinse your ear with clean, distilled water.
If it's a child battling an earache, do your best to get them comfortable by taking their mind off the pain.
You may want to:
If your child is of teething age, offer cooled teething toys for chewing.
This method also works for adults. Treat yourself to a good book or a favorite movie to take your mind off the earache.
There are many possible causes of earache. Possible causes that are relatively common include:
The most common ear infection is acute otitis media (AOM), or a middle ear infection.
It's characterized by swollen and infected portions of the middle ear. The pain associated with AOM is caused by fluid becoming trapped behind the eardrum. Symptoms may include:
Babies and children may be restless, cranky, and pull at their ears.
The best home remedy for an earache depends on the cause. If a cavity is to blame, your earache may not improve until you see a dentist. However, if it's an ear infection, using a natural remedy could make the illness bearable as your body fights off the infection.
Be sure to check with your child's pediatrician if your child has ear pain, especially if they are under 2 years of age.
If your child is running a high fever, or if a fever lasts longer than a day, seek immediate medical care. High fever for children is defined as:
Your doctor can provide guidance on whether you should try home remedies first or consider an antibiotic.
How do you get rid of an earache fast?There's no immediate magic cure for earache, but some natural or over-the-counter remedies can provide relief. Depending on the cause, you may need to get medical treatment.
When should I go to the doctor for earache?Any time there's ear pain, it's a good idea to see a doctor to find the cause and see if you need treatment. That said, if your pain is mild, you can try to wait a bit and see if it resolves on its own. Definitely see a doctor if your pain is acute or you also have a fever.
How long should an earache last?Many ear infections clear up on their own in about a week or two, with symptoms starting to get better after a few days. However, if your pain has another cause, it may resolve sooner or later. If the pain hasn't resolved within several days, make an appointment with your doctor.
While there isn't much evidence on alternative treatments for earaches, many home remedies can soothe the pain.
No Need For Antibiotics The latest guidelines from the AAP suggest that doctors should focus on pain management, not antibiotics, for ear infections. This is because ear infections often go away on their own, and the overuse of antibiotics could lead to antibiotic-resistant infections.
Why Does My Ear Hurt When I Swallow?
There are many things that can cause pain in the ear while swallowing. In many cases, it's likely due to an ear or throat infection.
Ear pain comes in many different shapes and sizes. Sometimes it throbs for hours. Sometimes it only hurts when you touch it.
In other cases, it might only show up when you're doing something that doesn't involve your ears, such as swallowing. Keep reading to learn more about the common causes of ear pain when swallowing, and how you can treat them.
A common cause of ear pain when swallowing is an ear infection. Most ear infections are caused by a bacterial or viral infection in the middle ear. They usually cause swelling, fluid buildup, and irritation inside your ear, which can cause pain.
Ear infections are common in children, but adults can also get them. When you get an ear infection as an adult, the symptoms may be slightly different than they were during your childhood.
Middle ear infectionMiddle ear infections, also called acute otitis media, are the most common. They affect the space behind your eardrum. That air-filled space contains small, vibrating bones that allow you to hear. It's connected to your throat by a pair of narrow tubes called Eustachian tubes.
Most ear infections are started by another condition, such as a cold, flu, sinus infection or allergies. The Eustachian tubes normally drain fluid from the middle ear. When you're congested, your Eustachian tubes can clog up. The fluid that accumulates around the blockage can become infected.
The Eustachian tubes are also responsible for maintaining pressure in the middle ear. When you swallow, yawn, or sneeze. The tubes open up to release pressure, which can be painful in an infected ear.
Signs of an ear infection in young children can include:
Adults with a middle ear infection may experience:
Many middle ear infections improve on their own within one week. Certain children may benefit from oral antibiotics, but they're often unnecessary, particularly in adults.
Swimmer's earSwimmer's ear is a type of otitis externa or outer ear infection. It's a different type of ear infection that affects your outer ear. When you swim or take a shower, water can fill your ear canal. This creates a warm, moist environment that's ideal for bacteria and fungus to grow.
An outer ear infection isn't always caused by water. Germs can also enter the ear canal through a foreign object, such as your finger. Q-tips and fingernails can injure the delicate lining of the inner ear that protects it from infection. Skin conditions, such as eczema, can also make a person more prone to this type of infection.
Pain from an outer ear infection often gets worse when the ear is tugged or stretched. The pain may become more intense when you're chewing and swallowing. The pain can radiate throughout the affected side of your face.
Other symptoms of an outer ear infection include:
This infection usually clears up after 7 to 10 days of medicated ear drops. Over-the-counter pain relievers can help to reduce the pain while you recover.
Although ear infections are a common cause of ear pain, they sometimes begin as nose or throat infections.
Children can develop complications from nose and throat infections because of the activity of their immune system.
Children have small pads of immune tissue called adenoids at the back of their nasal passages near the Eustachian tubes. The adenoids play an important role in the immune system of children. Adenoids are largest during childhood and typically shrink down by early adulthood.
The adenoids work by reacting to germs that enter through the mouth and nose. Sometimes, adenoids can become so large in response to an infection, that they block the Eustachian tubes, leading to middle ear infections.
TonsillitisTonsillitis is inflammation and infection of the tonsils, typically caused by a throat infection. The tonsils are two round pads of immune tissue at the back of your throat.
The main symptom of tonsillitis is a sore throat, but it can also cause:
The most common cause of tonsillitis is a bacterial infection. The same bacteria that causes strep throat (group A Streptococcus) causes most tonsillitis. Tonsillitis typically responds well to antibiotics.
Peritonsillar abscessA peritonsillar abscess is a collection of pus around one of your tonsils. It's usually a complication of untreated tonsillitis. The pain is often quite severe and distinctly worse than a regular sore throat. Only one tonsil is usually affected, which means the pain is worse on one side than the other.
A peritonsillar abscess often causes pain in the ear of the affected side. The pain when swallowing may feel unbearable. You might also have pain when opening your mouth.
Minor surgery is often necessary. Doctors treat the abscess by making an incision or using a small needle to drain the pus. Your doctor may also prescribe a course of antibiotics to treat the underlying tonsillitis and prevent the abscess from coming back.
Eagle syndromeEagle syndrome is a rare disorder that causes recurring pain in the back of the throat and the face. The throat pain is usually dull and persistent and often radiates to the ear. The pain gets worse when you move your head.
Other symptoms include:
Eagle syndrome is caused by problems with the ligaments and small bones of the neck or skull. It usually requires surgery to correct the problem.
Glossopharyngeal neuralgiaGlossopharyngeal neuralgia (GPN) is another rare condition that can be extremely painful. It involves a nerve of the head and neck known as the glossopharyngeal nerve. GPN is characterized by short, intense episodes of stabbing pain that are often triggered by cold liquids, swallowing, yawning, talking, coughing, or chewing. The pain is often focused around one ear, but can also include the tongue, back of the throat, face, or under the jaw.
GPN episodes usually last about two minutes and are followed by a period of dull aching. Treatment for GPN often involves prescription medications designed to treat neuropathic pain, such as pregabalin and gabapentin. Surgery may benefit those not helped by medications.
Temporomandibular joint dysfunctionTemporomandibular joint (TMJ) dysfunction affects the joint that you use every time you open or close your mouth. The joint is where your jaw bone connects to your skull.
A small disk of cartilage on each side of the joint separates the bones of your jaw from your skull, and allows them to glide easily when you swallow, talk, or chew.
Because you use this joint so often, damage can lead to considerable pain. Many people feel this pain in their ears as well.
Other symptoms of TMJ problems include:
There are several ways to damage the TMJ, including trauma, teeth grinding, and excessive gum chewing. Treatment typically involves lifestyle changes, rest, and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin).
While ear and throat infections may improve on their own within a week, you may need prescription medication. If the pain doesn't go away, contact your doctor to make sure it's not a sign of another underlying condition.




Comments
Post a Comment